Plantar Fasciitis
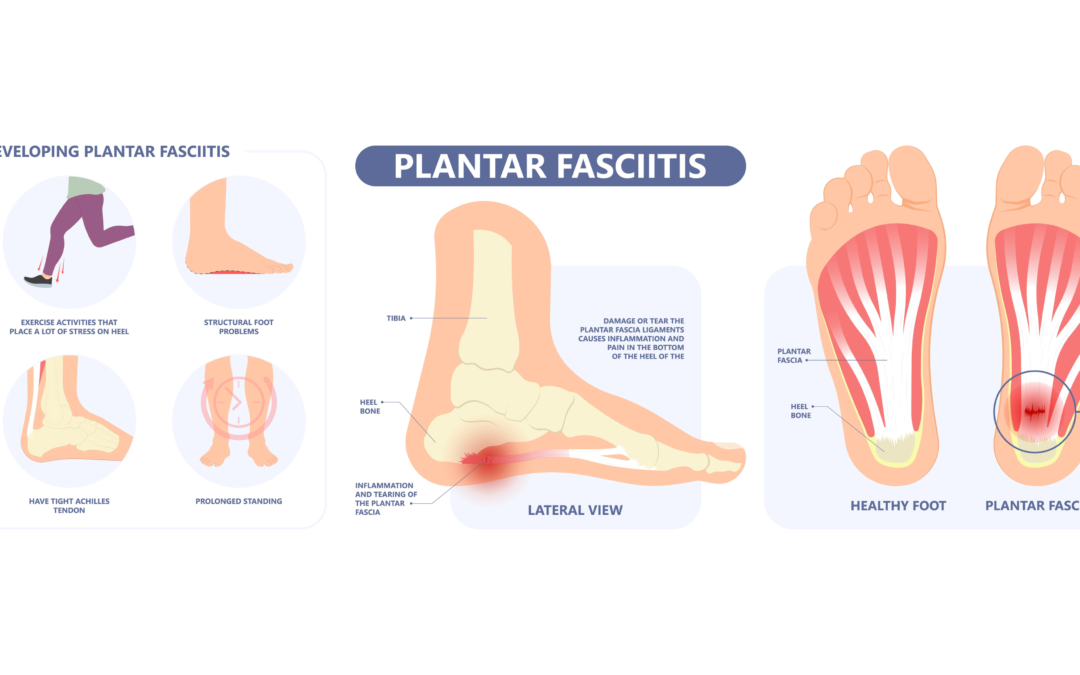
Most of us know someone who has complained about their foot hurting. Plantar fasciitis is the most common cause of foot pain affecting close to 2 million people each year, according to the American Academy of Orthopedic Surgeons (AAOS). Plantar fasciitis is inflammation, or tearing of the tissue on the bottom of our feet called the plantar fascia. This tissue is solid and is designed to withstand significant pressure, like from the many activities we enjoy, such as running or jumping. Sometimes we exert too much pressure on that tissue, leading to tearing, inflammation, and ultimately pain.
What causes plantar fasciitis?
- Many factors can lead to someone developing plantar fasciitis; here are just a few of the risk factors:
Tight muscles/joints – Most notably the calf muscles, as they can limit the amount of dorsiflexion in the ankle (bringing the foot up), a significant risk factor. Tightness or limitations in other areas, such as the hamstrings or hip flexors, should also be considered. - Biomechanical – The structure of our foot can play a significant role in causing plantar fasciitis. Most commonly, either a low arch (pes planus) or a high arch (pes cavus) can place abnormal stress on the tissue. Pronation is a normal motion where the foot becomes a shock absorber by “unlocking” and conforming to the ground to absorb impact. Sometimes the foot can overpronate, placing too much stress on the plantar fascia and leading to injury.
- Occupational – There is a link between prolonged standing/walking and the incidence of plantar fasciitis. Occupations that require long-standing, such as a machine operator, can put one at a higher risk of developing plantar fasciitis. A sudden change in the amount of stress placed on the foot, such as training on a rigid surface like a tennis court or a new footwear adaptation, can lead to plantar fasciitis.
What can I do to prevent or treat plantar fasciitis?
If you suspect that you may have plantar fasciitis, you can do a few things to accomplish two main goals: Reduce inflammation and stress on the tissue. Using ice on the area with a standard ice pack or a frozen water bottle can help control the inflammatory process and promote healing (tip: do not leave ice on longer than 15-20 minutes at a time**). The most common strategies for reducing tissue stress are prescribing proper footwear, taping, orthotics, and night splinting.
**If you have decreased sensitivity in the foot area due to diabetes or neuropathy, please seek the advice of your physician before beginning an icing regimen.**
Cray Physical Therapy has therapists who specialize in treating and managing plantar fasciitis. If you know of someone suffering from foot pain, please have them call us at 339-987-4856 so we can help them get on the road to recovery!